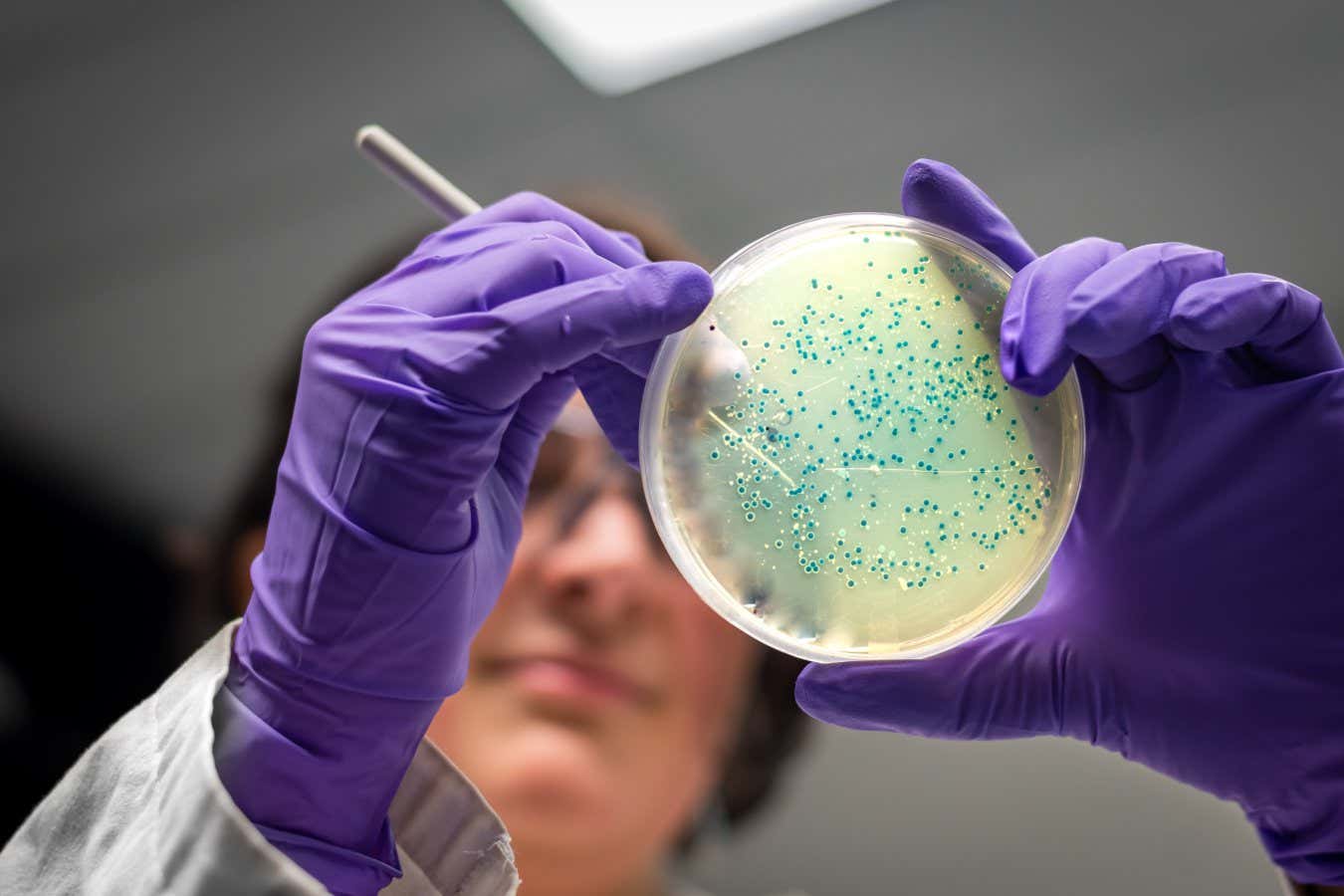

Some microbes have a growing resistance to our antibiotics
iStockphoto
The number of global deaths directly attributable to antibiotic-resistant bacterial infections is forecast to rise from a record 1.27 million a year in 2019 to 1.91 million a year by 2050. In total, antibiotic resistance is expected to kill 39 million people between now and 2050 – but more than a third of that toll could be averted if we take action.
Resistance occurs when microbes evolve the ability to survive drugs that were deadly to them, meaning they no longer clear up infections. Because of the widespread use of antibiotics, in farming as well as healthcare, a growing number of microbes are becoming resistant and spreading globally, but the full scale of the problem is unclear.
To address this, Eve Wool at the Institute of Health Metrics and Evaluation (IHME) in Seattle and her colleagues have tried to estimate the annual number of deaths due to antibiotic resistance from 1990 to 2021. “Our estimates are based on more than 500 million records,” says Wool. “We have a lot of coverage geographically and across time.”
While the overall number of fatalities due to this has been rising, the team found that the figure for young children has been falling as a result of vaccinations and improved healthcare. Between 1990 and 2021, deaths due to antibiotic resistance decreased by more than 50 per cent among children younger than 5, compared with a rise of more than 80 per cent in adults over 70.
Overall, deaths attributable to antibiotic resistance rose from 1.06 million in 1990 to 1.27 million in 2019 and then fell to 1.14 million in 2021, the team concludes. However, the decline in 2020 and 2021 is thought to be a temporary blip caused by covid-19 control measures reducing other kinds of infections, too, rather than to a lasting improvement in combatting resistance.
In the study’s “most likely” scenario for the decades to come, deaths from antibiotic resistance rise to 1.91 million a year by 2050. In a scenario in which new antibiotics are developed against the most problematic bacteria, 11 million deaths would be averted between now and mid-century. In a “better care” scenario where more people also have access to good healthcare, even more deaths are avoided.
The 1.91 million annual deaths figure is much lower than an often cited one of 10 million deaths in 2050, from a 2016 review. That forecast was based on less reliable estimates and also included the problem of resistance to non-antibiotic drugs in diseases such as HIV and malaria, says team member Mohsen Naghavi, also at the IHME.
The new study is more thorough than previous efforts, says Marlieke de Kraker at Geneva University Hospitals in Switzerland, but still has some major limitations. For instance, it assumes the risk of antibiotic resistant infections causing deaths is the same around the world, when this isn’t the case. “If basic healthcare infrastructure is limited, drug-resistant infections do not necessarily lead to more deaths than drug-susceptible infections,” says de Kraker.
She is also sceptical about the team’s forecasts. “I feel predicting antimicrobial resistance trends is very unreliable,” says de Kraker. Drug-resistant versions of microbes can suddenly emerge or disappear without experts really understanding the underlying mechanisms, and there are frequently black swan events, which are impossible to predict, she says.
Topics:






